February assessment
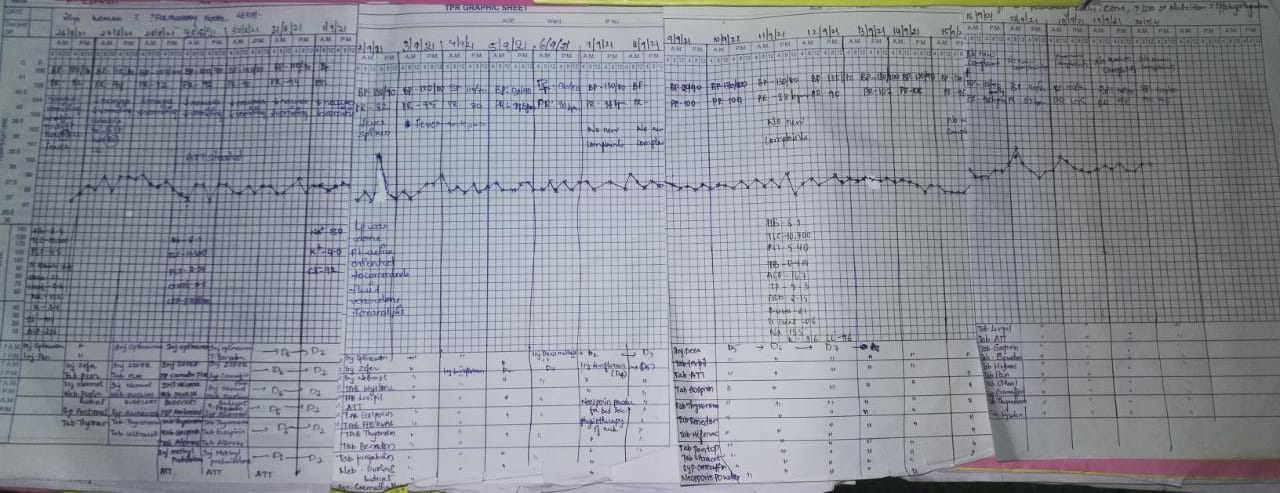
50 year man, he presented with the complaints of
Frequently walking into objects along with frequent falls since 1.5 years
Drooping of eyelids since 1.5 years
Involuntary movements of hands since 1.5 years
Talking to self since 1.5 years
More here: https://archanareddy07.blogspot.com/2021/02/50m-with-parkinsonism.html?m=1
Case presentation links:
https://youtu.be/kMrD662wRIQa). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?Ans) problem presentation:drooping of eyelids since 8 to 9 months refractory to treatmentinvoluntary movements of bilateral upper limbsfrequent episodes of fatigue since one yearthin stream of urine with bed wetting since one yearaccording to attenderschange in behavior (talking to self) since 1.5 yearsanatomical localisation of lesionb/l ptosis-weakness of levator palbebral superioris(without loss of frowning)self talk-frontal lobevertical gaze palsy:the centres and pathway for vertical gaze:vertical gaze palsy issupranuclearnuclearinfranuclear (eg.nmj disorders)the doll's eye manaever is used to differentiate between supra and belowsuggesting the activation of vestibulo -occular system which directly activates the thalamo-mesencephalic centre,therefore intact doll's eye, suggests a supranuclear lesionb) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.Ans) 1)mysasthenia gravis2)3rd nerve pasy3)horner's syndrome4)myotonic dystrophy5)kearnes syres(mitochondrial )6)occuplopharyngeal muscular dystrophy7)cerebral ptosis(other conditions to be correlated)The size of pupis being normal:rules out horner's or 3rd cn palsy(as a single nucleus supllies both levator palpebral superioris ,its lesion causing b/l ptosismysasthenia-no history of fluctuation/fatigueable ptosismyotinic dystrophy-no other signs of the disease, especially on sustained contraction of the musclesthe KS syndrome has age of onset before 20occulo pharngeal-intact bulbar cranial nerves rules this out.self talking and altered behavior-frontal lobe of the brain.Frequent falls.following clinical examinationcereballar lesions can be ruled outnmj disorders- no history of fluctuation,pain,tone and power normal on examinationthe differential of basal ganglia disorders can be derivedand loss of vertical gaze can lead us to suspect progressive supranuclear palsy(confirmed with imaging)c)What is the efficacy of each of the drugs listed in his current treatment planAns) syndopa was initiated to differentiate psp from Parkinson's diseasehttps://www.nejm.org/doi/full/10.1056/nejmoa033447In this randomized, double-blind, placebo-controlled trial, we evaluated 361 patients with early Parkinson's disease who were assigned to receive carbidopa–levodopa at a daily dose of 37.5 and 150 mg, 75 and 300 mg, or 150 and 600 mg, respectively, or a matching placebo for a period of 40 weeks, and then to undergo withdrawal of treatment for 2 weeks. The primary outcome was a change in scores on the Unified Parkinson's Disease Rating Scale (UPDRS) between baseline and 42 weeksThe severity of parkinsonism increased more in the placebo group than in all the groups receiving levodopa: the mean difference between the total score on the UPDRS at baseline and at 42 weeks was 7.8 units in the placebo group, 1.9 units in the group receiving levodopa at a dose of 150 mg daily, 1.9 in those receiving 300 mg daily, and –1.4 in those receiving 600 mg daily (P<0.001)2) More here: https://ashfaqtaj098.blogspot.com/2021/02/60-year-old-male-patient-with-hrref.html?m=1Case presentation links:https://youtu.be/7rnTdy9ktQwa) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?Ans) problem representation:progressive sob from grade 2 to 4 since 2 monthsorthopnea,pndb/l pedal edema upto knee since 2 monthsGeneralised weakness since 2 monthsH/o cva (rt hemiparesis recovered) with persistent loss of speech since 2 years.anatomical localisationbased on history:pnd ,sob with orthopnea suggest left heart failurebased on examination:shift of apex to 6th ics,presence of thrill palpable at apex(?s1), nature of the apex not mentionedpresence of loud p2 ,dilated veins ,pedal edema,s3 in both apical and left parasternal areas.(?biventricular failure)b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.etiology:CADEcg showing1)normal axis2)pathological Q waves from v1 to v63)poor R wave progressionsuggest a CAD probably involving LAD and LCX territoryconfirmed with finding on the echo1)heart failure in the setting of CAD occurs due tomyocardial infarction (MI) frequently leads to permanent death of cardiac muscle. The infarcted segment is akinetic/dyskinetic, thus leading to inadequate relaxation in diastole and impaired contraction in systole2)subsequent remodeling of the ventricle can occur in myocardial segments that are remote from the site of infarction. Such regional remodeling frequently results in a distortion of ventricular structure and geometry, and can contribute to a further decline in ventricular function . Ventricular dilatation can promote annular dilation, with consequent mitral regurgitation, which can predispose to heart failure.C) What is the efficacy of each of the drugs listed in his current treatment plan1)salt and fluid restrictionhttps://pubmed.ncbi.nlm.nih.gov/23787719/#:~:text=Conclusion%3A%20Individualized%20salt%20and%20fluid,Quality%20of%20life%3B%20Salt%20restriction.Ninety-seven stable patients in NYHA class II-IV, on optimal medication, with previous signs of fluid retention, treated with either >40 mg (NYHA III-IV) or >80 mg (NYHA II-IV) of furosemide daily were randomized to either individualized salt and fluid restriction or information given by the nurse-led heart failure clinics, e.g. be aware not to drink too much and use salt with caution, and followed for 12 weeks. Fluid was restricted to 1.5 L and salt to 5 g daily, and individualized dietary advice and support was given.Results After 12 weeks, significantly more patients in the intervention than in the control group improved on the composite endpoint (51% vs. 16%; P < 0.001), mostly owing to improved NYHA class and leg oedema. No negative effects were seen on thirst, appetite, or QoL2)benfomet as thiamine replacement in alcoholic ptshttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC4550087/33)aldactone(spironolactone)https://www.aafp.org/afp/2001/1015/p1393.htmlBased on earlier work suggesting a benefit of therapy,2 the Randomized Aldactone Evaluation Study (RALES) was undertaken to evaluate the role of spironolactone when used in addition to standard therapy for CHF. Standard therapy in this study did not include beta blockersS-The investigators prospectively enrolled 1,663 patients with severe (New York Heart Association [NYHA] class IV) CHF (Table 1).4 Most of the enrolled patients were white men averaging 65 years of age. These patients had a left ventricular ejection fraction of 35 percent or less and marked physical limitations related to CHF. Patients were excluded if they had unstable angina or moderate renal failure, and if they were hyperkalemic.All patients who could tolerate the drug were given an ACE inhibitor and a loop diuretic, and 70 percent were taking digoxin. Only 10 percent were taking beta blockers. Patients were randomly assigned to receive placebo or 25 mg of spironolactone daily in addition to their current regimen. After eight weeks, if the patient showed worsening CHF and had a stable potassium level, the dosage was increased to 50 mg daily. The dosage was decreased to 25 mg every other day if at any time the patient became hyperkalemic4)furosemide 80mg5)telmisartan 40mgQuestion 3More here https://soumya9814.blogspot.com/2021/01/this-is-online-e-log-book-to-discuss.html?m=1Case presentation video:https://youtu.be/40OoVEQBgS4a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?Ans: problem presentation:sob grade 2 or 3?non progressive since 10 dayscough with sputum since 10 daysdecreased sleep since 10 daysdecreased appetite since 10 daysafter admission:drowsiness and giddinessanatomical localisation:sob without pedal edema, pnd, orthopnea can be localised to the lung(sob on evxertion grade 2 can also be localised the heart but no history or examination finding of pedal edema or jvp rise rules it out)cough withb)What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.A)?Sub acute combined degeneration of spinal cord secondary to vit B12 deficiency.?Diabetic neuropathy?Hypervolemic hyponatremia secondary to heart failure?Pseudohyponatremia secondary to uncontrolled sugarsc) What is the efficacy of each of the drugs listed in his current treatment plan especially for his hyponatremia? What is the efficacy of Vaptans over placebo? Can one give both 3% sodium as well as vaptan to the same patient?A)https://www.sciencedirect.com/science/article/pii/S0085253815551089THE INDICATIONS FOR VAPTANS ARE NOT CLEAR1-First, we do not know how to distinguish between symptoms that are an indication for vaptan and those that are not.2-Together, we lack information on which degree of severity of hyponatremia should give us reason to consider vaptan treatment.3-Third, work by Gankam Kengne et al.28 suggested that patients with mild chronic hyponatremia fall to the ground more often than matched normonatremic controls .We are unable to answer the question of whether elderly patients with chronic mild hyponatremia should be treated, for example, by a vaptan to correct hyponatremia and prevent fractures.4-Fourth, in terms of indication for vaptan, the area least controversial might appear to be that of severe symptomatic (chronic) hyponatremia. A ‘hyponatremia-naive’ physician is likely to conclude that vaptans if anything should be promising in severe symptomatic hyponatremia. However, there are literally no published data on this. Clinical trials of vaptans have consistently excluded severe symptomatic hyponatremia from study because of ethical concerns (risk of worsening of severe symptoms when receiving placebo)recent expert panel suggested that in severe symptomatic (chronic) hyponatremia, infusions of hypertonic saline should have priority over vaptan.30 This is an area of significant uncertainty. It has been pointed out that 3% NaCl may correct hyponatremia too quickly,31 or it may occasionally lead to pulmonary edema in SIAD(H). On the other hand, we have personal experience (PAG) that SIAD(H)-related severe symptomatic hyponatremia is a rewarding indication for vaptan. Thus, in the absence of a trial comparing fluid restriction plus 3% saline with vaptans in severe symptomatic hyponatremia, we do not have a database to make specific recommendations for or against vaptans.4) Please mention your individual learning experiences from this month.Posted in ICU1) Learned about the ventilator settings2) Learned about the heart blocks in CKD pt3) MOA of tamsulosin in BPH4) Approch to sudden onset of sob in CKD patients5) CSF analysis6) Difference between traumatic tap and subarchnoid haemorrhage7) Management of hyponatremia8) Done 2 pleural Taps9) Learned about the procedure of lung biopsy