56/M with ulcer on right foot
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
Thank you Dr.Gouri
Acknowledged from https://gourireddy50.blogspot.com/2022/07/56m-with-ulcer-on-right-foot.html
Case :
A 56 year old male had come to the OPD with chief complaints of ulcer on the right foot since 18 days and rat bite on the right index finger since 10 days.
History of Present Illness :
Patient was apparently asymptomatic 18 days ago, then he developed a painless blister on the medial aspect of his right foot which eventually burst to form an ulcer.
For the first few days, the patient turned a deaf ear to the ulcer thinking it would get healed on its own. On Thursday (14th of July, 2022), on his way back home from work, he noticed watery discharge oozing out of the ulcer which was non foul smelling and non blood stained. After washing his foot, he noticed the skin over the ulcer chipping off. This was an alarming sign that had made him come to the hospital on Friday (15th of July, 2022).
10 days ago, in his sleep a rat bit him on the right index finger. Until the next morning, he had not noticed the bite.
Presence of ulcer on the plantar aspect of the left hand.
Daily Routine :
The patient is a lorry driver by occupation.
He wakes up at 5 AM in the morning and has his breakfast by 8 AM and leaves for work.
Usually has his lunch by 1 PM and Dinner by 8 PM. He has been drinking alcohol (90ml) everyday for the past 40 years now.
Past History :
Not a known case of Hypertension, Asthma, Epilepsy, Tuberculosis, Thyroid disorders.
The patient is a known case of diabetes type 2 since 7 years.
7 years ago, a blister was formed on the lateral malleolus of his left foot which he took no notice of. 4-5 days later, he started feeling giddy, tired and had downtime in his work. So he had been taken to the hospital and had been diagnosed with diabetes. He’s been on medication ever since.
Personal History :
Sleep : Normal
Diet : Mixed
Appetite : Normal
Bowel and Bladder Movements : Regular
Addictions : Patient consumes alcohol everyday since 40 years. Patient used to smoke beedi (1 pack a day) and cigarette (1 pack a day) since the age of 12. He has quit smoking since 2 years.
Family History :
No similar complaints
General Examination:
Pallor - absent
Icterus - absent
Cyanosis - absent
Clubbing of the fingers - absent
Lymphadenopathy - absent
Pedal Oedema - absent


Vitals :
Temperature - 98.4 degree Fahrenheit
Pulse - 86 bpm
Respiratory rate - 16 cpm
BP - 110/70 mm of Hg
Systemic Examination :
CVS - S1 and S2 were heard
Respiratory system - bilateral vesicular breath sounds are present
Abdomen - soft and non tender
CNS Examination:
Deep reflexes -
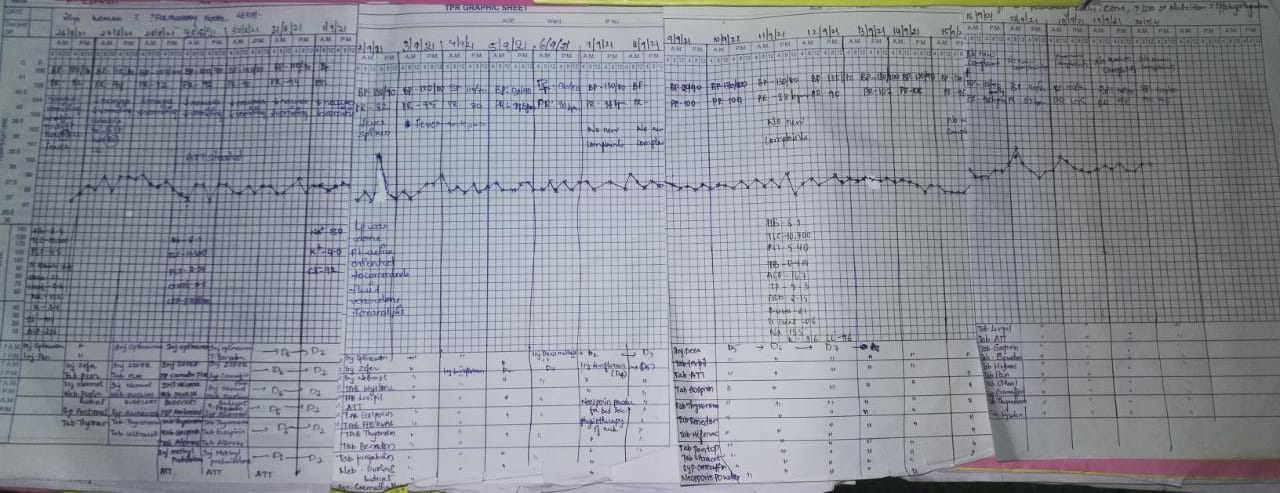
Investigations :
RBS -
[20/07/2022] 8 AM - 198 mg/dl ; 2 PM - 158 mg/dl ; 8 PM - 358 mg/dl
[21/07/2022] 8 AM - 193 mg/dl ; 2 PM - 384 mg/dl ; 8 PM - 282 mg/dl
[22/07/2022] 8 AM - not taken ; 2 PM - 185 mg/dl ; 4 PM - 240 mg/dl ; 8 PM - 
Provisional Diagnosis :
Diabetic ulcer on the right foot
Rat bite on right index finger
Treatment :
Tab Glimi M1 1/2tab OD
Tab Glimi M2 OD
Inj H Actrapid S.C GRBS 6th hourly
T Bact Ointment OD
T Fucid Cream OD
Discharge summary: